Starting this month, federal COVID vaccine policy has shifted in a big way—and it’s already affecting who can get boosted. While seniors and people at higher risk still have access, healthy adults, pregnant women, and kids are now facing unexpected roadblocks. Here’s what’s changed and what it means for you.

New Federal Covid Vaccine Rules Just Took Effect
| Insight | Stat |
|---|---|
| Only 23% of U.S. adults got the last booster | 2023–24 season |
| New FDA policy limits boosters to 65+, high-risk, and immunocompromised groups | May 2025 update |
| Pregnant women and children now need “shared decision-making” with providers | CDC guidance |
The government’s COVID vaccine playbook just got a major rewrite. It’s now more selective, more cautious—and, for many, more confusing. If you’re under 65 and healthy, you may need to wait or advocate harder to get a shot. For now, the best move is to stay informed and keep communication open with your healthcare team.
Why did the rules change?
In May 2025, the FDA overhauled how COVID vaccines are approved and recommended. Their new strategy focuses on people most at risk: those over 65, those with chronic medical conditions, and the immunocompromised.
If you’re not in one of those groups? You’ll now need to wait for new, trial-backed vaccine approvals—something that could take months or even longer. The FDA argues this new process avoids unnecessary vaccination, but critics say it cuts off access for many who still want the option.
“This isn’t about denying care,” an FDA spokesperson told The Washington Post. “It’s about targeting resources where they have the clearest benefit.”
Who’s now left out?
- Healthy adults under 65: No longer automatically eligible for new boosters.
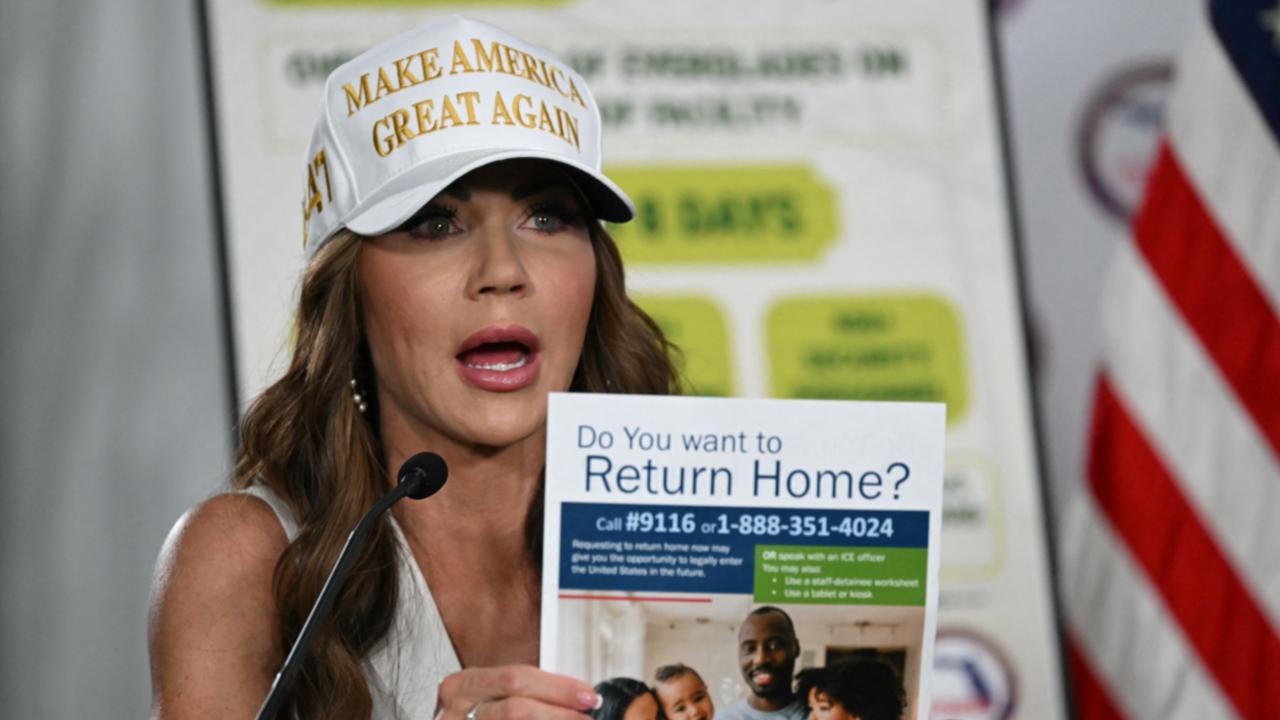
- Pregnant women: Previously prioritized, now advised to consult their doctors.
- Children and teens: Routine vaccination has been paused pending further data.
That means if you’re healthy and under 65, even with insurance, your pharmacy might turn you away unless you qualify under stricter conditions.
Real-life consequences: confusion and denied access
I saw this firsthand. A friend in her 30s with a chronic condition (but not one listed in the updated guidelines) was told by two pharmacies she “didn’t qualify” for a booster—even though her doctor recommended it. Stories like hers are becoming more common.
Doctors speak out: “We weren’t prepared”
Many healthcare providers say they were caught off guard by the policy switch. The American College of Obstetricians and Gynecologists issued a statement urging continued vaccination for pregnant patients, calling the new guidance “premature and risky.” Pediatricians agree.
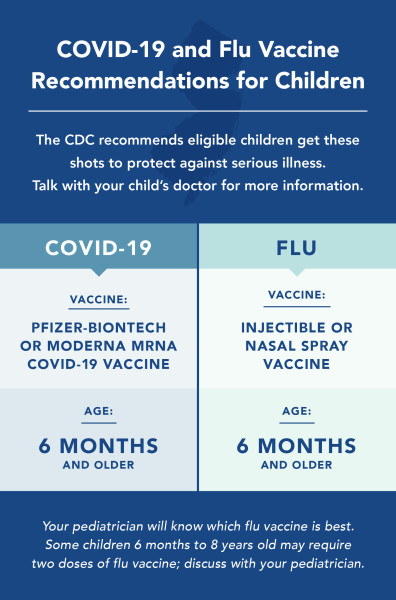
“There’s been no change in vaccine safety,” said Dr. Kristina Bryant, an infectious disease expert in Kentucky. “But the way these new rules were rolled out makes families question what’s safe—even when the data hasn’t changed.”
So, can you still get vaccinated?
That depends on your health status and your insurance plan. While the CDC’s immunization schedule still includes COVID vaccines, which usually guarantees coverage, the lack of a clear recommendation muddies things.
Here’s what to expect:
- 65+ or high-risk: You’re good to go. Walk into most pharmacies and you’ll still get the shot.
- Pregnant or parenting: You’ll need to talk to your provider first. Some insurers may require documentation.
- Healthy and under 65: It’s likely you’ll need to wait for new trial data and a revised CDC recommendation.
What’s next?
The CDC’s vaccine advisory committee (ACIP) is set to meet again later this month. They could recommend broader coverage or clarify insurance expectations. Meanwhile, Moderna and Pfizer are preparing new trials aimed at younger, healthy adults—though updated shots likely won’t be available until 2026.
“This is a holding pattern,” said Dr. Paul Offit, a top vaccine advisor. “We’ve chosen to slow the rollout for healthy people while we collect more data. That’s scientifically cautious, but it’s also frustrating.”
What you can do now
- Talk to your provider. Especially if you’re pregnant, immunocompromised, or have kids.
- Check your insurance plan. Some will still cover off-label vaccines if your doctor signs off.
- Watch for CDC updates. Guidance may change quickly depending on public reaction and new data.
FAQs
Why did the FDA limit vaccine eligibility?
The agency wants to prioritize groups most likely to benefit from boosters, such as the elderly and those with medical vulnerabilities.
Are COVID vaccines still safe for pregnant women and kids?
Yes, according to major medical associations. But federal agencies now leave that choice to patients and their doctors.
Will insurance still pay for a vaccine that’s not “recommended”?
Probably. COVID shots remain on the CDC’s immunization schedule, which most insurance plans follow for coverage.
When will healthy adults get access again?
Possibly in 2026, once new trial data supports broader approvals. Some mid-season authorizations could arrive earlier for adults over 50.